All Your Eye Care And Eyewear
in One Place
Missouri Eye Consultants are your local eye experts. We’re dedicated to helping you see clearly and comfortably — no matter what attention your eyes need.
About Missouri
Eye Consultants
We have been your family’s trusted resource for every eye care need for more than 60 years: first as Columbia Eye Consultants Optometry, and now as Missouri Eye Consultants. As we’ve grown and brought on new doctors, we’ve always held fast to our belief in offering a full range of services so that no matter what ails you, we can customize your care to keep you seeing clearly.
You shouldn’t have to travel far for exceptional eye care. That’s why we provide it right here in your backyard! We are proud to be members of the communities we serve across Missouri. We live here, we work here, we’re neighbors — and we want to make sure you’re able to enjoy life’s beautiful sights.
Complete, Compassionate Eye Health Services
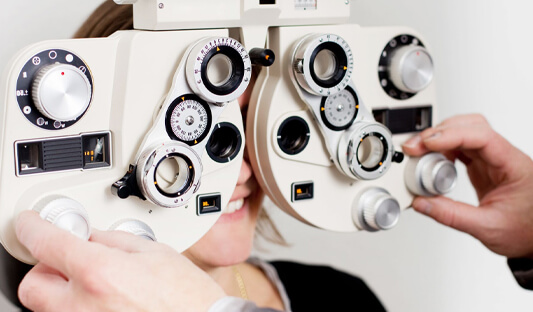
Comprehensive Eye Exams
Our diagnostic technology and know-how help you stay ahead of eye diseases.
Myopia Management
We can both correct nearsightedness and stop it from progressing.
Glaucoma Management
Our experts identify and treat glaucoma before it affects your vision.
Pediatric Eye Exams
Young eyes have unique needs — we know how to find and address them.
Cataract Surgery
Our specialist surgeons correct cataracts to restore your clear eyesight.
Dry Eye Management
Dry eye is uncomfortable, but we can offer fast and lasting relief.
In addition to these services, we also offer: contact lens exams, blue light protection, emergency eye care, LASIK and refractive surgery co-management, diabetic eye care, macular degeneration management, and much more!
Our Optical Selection
Glasses And Frames
No matter your needs, style, or budget, we can find the perfect frames for you. From classic and timeless to fashion-forward, our passionate opticians will help you find a pair you’ll love.
Contact Lenses
Contact lenses require a special eye exam to bring you an accurate fit and precise vision. Our team prides itself on taking their time during fittings to give our patients the best vision possible.
Sunglasses
Your eyes need protection from the sun’s harmful UV rays, and we’re here to help you do so in style with a great range of prescription and non-prescription sunglasses, from popular designers.
Why Choose Missouri Eye Consultants?
Your vision is too important to trust to just anyone. We’re proud to employ only the most caring and dedicated team members in Missouri. Our experienced staff use the latest proven technologies to monitor your eyes and take care of any potential issues.
Our team believes in taking care of our community — that’s why we dig a little deeper when it comes to taking care of our patients’ eyes. We’re dedicated to helping everyone see more clearly with customized care, and willing to go the extra mile to help our neighbors, no matter how complicated their needs.

Community Engagement
We love being a part of the communities we work and live in, so we want to give back — that’s why we’re the proud provider of eye care services and products for Mizzou’s student-athletes. We appreciate the hard work of these young people and want to help them focus on their performance in the classroom and in competition.
We also participate in the KindSight 2020 program, providing glasses to patients in Guatemala who need them. When you buy a pair of glasses at Missouri Eye Consultants, we donate a pair to be brought to Guatemala on our next mission trip!
![]()
![]()

Join Our Team
As a member of the Missouri Eye Consultants team, you’ll have access to state-of-the-art facilities and advanced technology, enabling you to deliver the highest standard of care. You’ll work in a supportive work environment that will not only enhance your skills and knowledge but also allow you to make a meaningful impact in the lives of patients in Missouri. We look forward to meeting you!
Meet Our Team
Our doctors take their time to understand your eye health and customize solutions for your personal needs. Their experience is only matched by their passion for their work — and your vision!
7 Convenient Locations
for All of Your Eye Care Needs
We’re here to provide the same excellent service and care at any of our seven convenient offices.